General Plastic Surgery
1. What are stem cells?
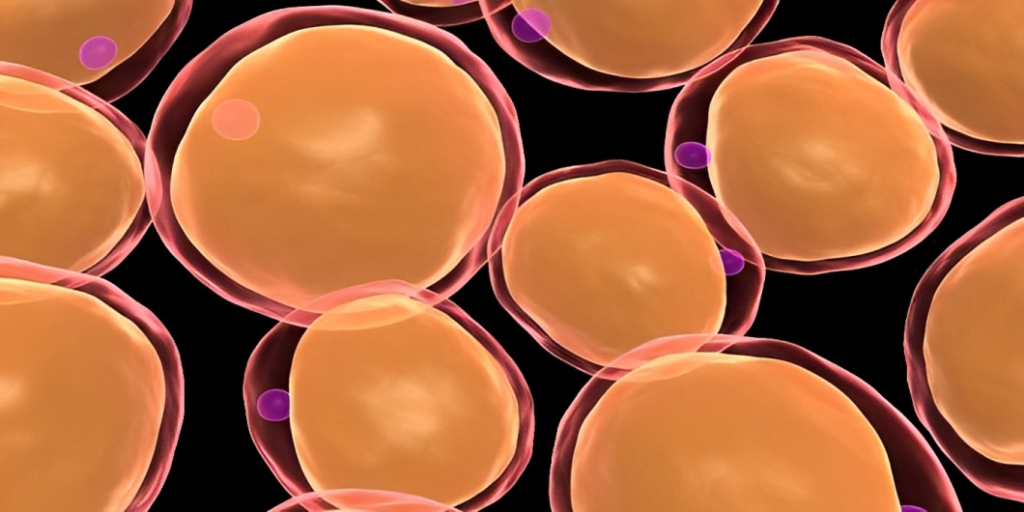
Stem cells are cells that have the remarkable potential to develop into many different cell types in the body during early life and growth. In addition, in many tissues they serve as a sort of internal repair system, dividing essentially without limit to replenish other cells as long as the person or animal is still alive. When a stem cell divides, each new cell has the potential either to remain a stem cell or become another type of cell with a more specialized function, such as a muscle cell, a red blood cell, or a brain cell.
Stem cells are distinguished from other cell types by two important characteristics. First, they are unspecialized cells capable of renewing themselves through cell division, sometimes after long periods of inactivity. Second, under certain physiologic or experimental conditions, they can be induced to become tissue- or organ-specific cells with special functions. In some organs, such as the gut and bone marrow, stem cells regularly divide to repair and replace worn out or damaged tissues. In other organs, however, such as the pancreas and the heart, stem cells only divide under special conditions.
2. Why Adipose (Fat) Derived Adult Stem Cells?
Adipose tissue ASCs (AT-ASCs) are extremely similar to stem cells isolated from bone marrow (BMSCs). The use of Stem Cells derived from fat or adipose tissue is a unique and promising approach and holds key advantages over stem and regenerative cells from other sources. While stem and progenitor cells usually make up less than 5% of all ADSCs, this is 2,500-fold more than the frequency of such cells in tissues such as bone marrow (0.002%). The abundance of ADSCs in adipose tissue and the ability to easily collect large amounts of adipose tissue via liposuction eliminates the need for tissue culturing.
Adult Stem Cells (ASCs/ ADSCs), by definition, are unspecialized or undifferentiated cells that not only retain their ability to divide mitotically while still maintaining their undifferentiated state but also given the right conditions, have the ability to differentiate into different types of cells including cells of different germ-origin – an ability referred to as transdifferentiation or plasticity.
Though the exact mechanism of transdifferentiation of ADSCs is still under debate, this ability of ADSCs along with their ability to self-renew is of great interest in the field of Regenerative Medicine as a therapeutic tool in being able to regenerate and replace dying, damaged or diseased tissue.
Clinically, however, there are a few criteria that ADSCs need to fulfill before they can be viewed as a viable option in Regenerative Medicine. These are as follows
- Abundance in numbers (millions to billions of cells)
- Ease of harvest (through minimally invasive procedures)
- Ability to differentiate into multiple cell types (which can be regulated and reproduced in vitro)
- Safe to transplant to a different site of the autologous host or even an allogenic host.
- No conflict with current Good Manufacturing Principles (during procurement, culture or transplantation)
3. Where are ADSCs obtained?
Compared to any other source, the vast amounts of adipose tissue (depots of fat for storing energy) especially in the abdominal region, by sheer volume of availability, ensure an abundance in numbers of ADSCs ranging in the millions per unit volume. The sheer numbers available also has the added advantage of not needing to be cultured in a laboratory over days in order to get the desired number of ADSCs to achieve what is called “therapeutic threshold” i.e. therapeutic benefit. In addition, harvesting ADSCs from adipose tissue through simple, minimally invasive liposuction under local anesthesia is relatively easier, painless and poses minimal risk to the patient compared to all other possible methods. Vaser Liposelection yields a higher number of stem cells than traditional Liposuction.
Clinically AT-ASCs have the advantage over their bone marrow-derived counterparts, because of their abundance in numbers – eliminating the need for culturing over days to obtain a therapeutically viable number – and the ease of the harvest procedure itself – being less painful than the harvest of bone marrow. This, in theory, means that an autologous (from the same patient) transplant of adipose-derived ASCs will not only work in much the same way as the successes shown using marrow-derived mesenchymal stem cell transplant, but also be of minimal risk to the patient.
AT-ASCs, like BM-ASCs, are called Mesenchymal ASCs because they are both of mesodermal germ-origin. This means that AT-ASCs are able to differentiate into specialized cells of mesodermal origin such as adipocytes (fat cells), fibroblasts, myocytes (muscle cells), osteocytes (bone) and chondrocytes (cartilage). AT-ASCs are also able to, given the right conditions of growth factors, transdifferentiate into cells of germ-origin other than their own. Animal model and human studies have shown AT-ASCs to undergo cardiomyogenic, endothelial (vascular), pancreatic (endocrine), neurogenic, and hepatic trans-differentiation , while also supporting haematopoesis (blood cells formation).
4. How do Stem Cells Work?
Autologous adult stem and regenerative cells are thought to promote healing of scarred or injured tissue. It is believed that this heterogeneous population of cells influences the local environment via cell-to-cell signaling, immune modulation, and differentiation into other cell types. In Cosmetic Applications, they are believed to help the transplanted fat survive better.
In addition, the extracellular matrix of harvested adipose tissue contains different types of Collagen such as Types 1, 3-4, 7, 14-15, 18 and 27 to name a few. This is important, in Fat Transfer protocol where freshly isolated fat is used as a filler in breast, buttock, or face augmentation or post-lumpectomy reconstruction of the breast and in the augmentation of the penis, and where collagen provides the structural support required for cell survival.
Furthermore, the extracellular matrix plays an important role in adipocyte endocrine secretions, and release of growth factors such as transforming growth factor beta (TGF-ß), platelet-derived growth factor (PDGF), and fibroblast growth factor (FGF), among others all of which are contained in what is called the Stromal Vascular Fraction (SVF). The SVF also contains the various proteins present in the adipose tissue extracellular matrix of which Laminin is of interest due to its ability to help in neural regeneration.
The cellular composition of the SVF ranges from pre-adipocytes to endothelial cells, smooth muscle cells, pericytes, fibroblasts, and AT-ASCs. Typically, the SVF also contains blood cells from the capillaries supplying the fat cells. These include erythrocytes, B and T cells, macrophages, monocytes, mast cells, natural killer (NK) cells, hematopoietic stem cells and endothelial progenitor cells, to name a few. The latter two types of cells, namely the hematopoietic stem cells and endothelial progenitor cells play important roles in supporting the viability of existing blood vessels and helping create new ones respectively.
These other ingredients that make up the SVF ‘cocktail’ act as an adjuvant to further augment the effect of the autologous transplant of SVF AT-ASCs.
Brief methodology for the Adipose derived Stem Cell therapy:
5. Are there any adverse reactions?
Autologous transplant of SVF AT-ASCs also poses extremely low risk to the patient when done as a single procedure in a sterile surgical operating room setting. Furthermore, it is postulated that SVF AT-ASCs due to their immunosuppressive properties may be transplanted into not only autologous but also allogenic tissues without initiating a cytotoxic T-cell response. However, Autologous transplants are believed to be the safest and most viable option at this point.
6. What are they used for?
Stem Cell or SVF therapy is still in its infancy. The use of stem cells in the treatment of many different medical conditions (including cardiovascular disease, soft tissue defects, wound healing, neurologic conditions and many more) is being evaluated in numerous clinical and preclinical studies around the world.
In Cosmetic surgery the stromal Vascular fraction (SVF) which includes AT-ASCs are mixed with fat taken from the patient’s donor area, and is then grafted or transplanted to the donor site, such as the breast. This results in most of the grafted fat surviving in its new host area. The other stem cells and growth hormones present in the SVF are believed to help enhance new capillary growth as well, helping the fat cells survive. This is called Cell-Assisted Lipotransfer, or CAL. There are numerous studies going on around the world to show that CAL is safe, easy, and superior to using implants as there are fewer complications.
Conventional breast augmentation procedures include fat injection, hyaluronic acid (Filler) injection, and breast Implants. In CAL, stem cells collected from the patient’s own adipose are concentrated and re-injected together with the fat. Because transplanted stem cells differentiate into new adipose tissue or vascular endothelial cells, this procedure has the advantages of a much higher fat graft survival (retention rate) and longer survival compared with common fat injection. Because of the use of the patient’s own adipose tissue, this represents a safer treatment with no concern for rejection or the other drawbacks of using implants. Other areas similarly treated by Fillers such as the cheeks, buttocks, etc can now be treated By CAL, leading to permanent, hassle-free improvements. SVF-Stem Cell Therapy is also undergoing intense research for the treatment of Baldness. Currently, Plant-based Stem cells are being injected into the scalp, both before and after Hair transplant, in order to stimulate new hair growth, and its use is showing promising results. In theory,however, autologous CAL should provide even better results for hair loss. SVF-Stem Cell Therapy is also being investigated for its role in anti-ageing and rejuvenation therapies, since intravenously (i.v) injected SVF travels in the bloodstream and repairs and heals all tissues that are damaged by trauma, disease or just wear-and tear due to age.
Our Contact Details
Consultation
Consultation Rooms: D.R.S. Medical Centre, Suite No. 98, 9th Floor, Lady Ratan Tata Institute, Indian Cancer Society Building,
M. Karve Road , Cooperage, Mumbai – 400021.
Timings: Monday – Friday: 2pm to 6 pm
Breach Candy Hospital, Warden Road, Mumbai
Timings: Tuesday – 7 pm to 8 pm only
